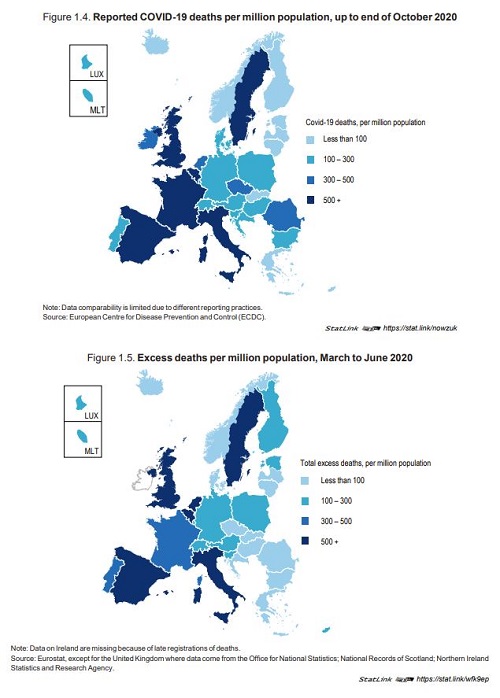
Since late 2019, the COVID‑19 outbreak has spread to become the most serious pandemic in a
century. European countries have been severely affected, with over 7 million cases and 220 000
deaths reported across EU countries, Iceland, Norway, Switzerland and the United Kingdom as of
31 October 2020. As the pandemic continues through 2020 and beyond, the eventual death toll will
rise.
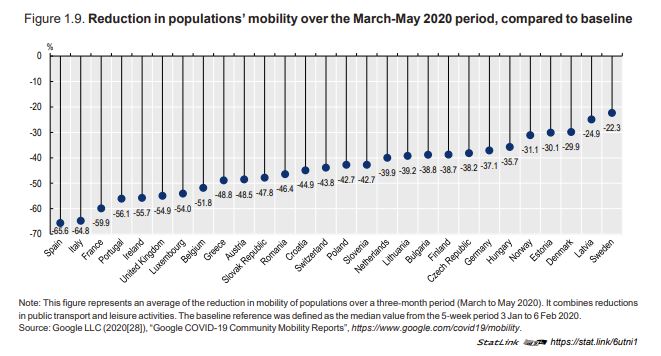
From the onset of the pandemic until the end of October 2020, non-medical containment and
mitigation actions were the only policy options countries had to prevent the spread of COVID‑19.
The majority of European countries implemented similar containment and mitigation measures during the first wave of the pandemic.
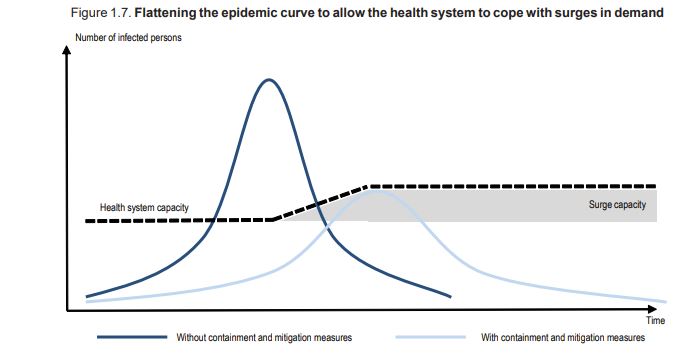
Containment and mitigation strategies aim to minimise the risk of transmission of infections and
slow the spread of the virus. Without any intervention, the spread of a viral infectious disease generally
follows an S-shaped curve. That is, infections grow slowly at the beginning of the outbreak, accelerate
exponentially in its central phase when a critical mass of people are infected and many others are still
susceptible, and slow in its final phase when enough people are immune (either through natural
infection or vaccination). The central phase of this cycle corresponds to the peak of the infection. The
different policy options described in this section aimed to prevent the COVID‑19 outbreak from
reaching its exponential acceleration phase, or to at least curb it to alleviate the burden on health care
systems (Figure 1.7).
Containment and mitigation strategies can be grouped into three broad policy categories with social distancing measures implemented in almost all European countries, but with
different levels of stringency
- Social distancing measures, notably: closing workplaces and non-essential services; school closures; banning mass gatherings; travel restrictions; and full society lockdowns.
- Improved personal and environmental hygiene, including the use of personal protective equipment such as face masks.
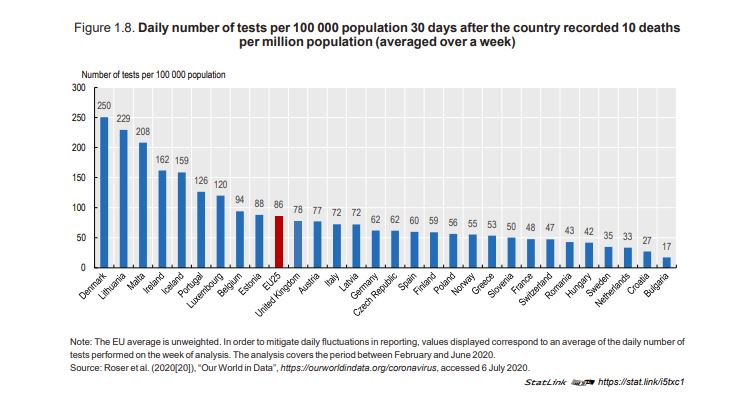
- Testing, tracking and tracing of infected individuals, with confinement of affected persons.
This can be targeted or more large-scale testing and quarantine policies.
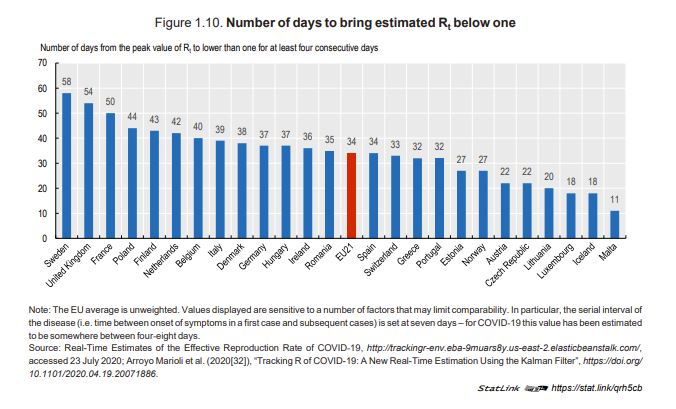
It took on average 34 days to European countries to control the first wave of the outbreak. The effectiveness of containment and mitigation strategies depends on the rapidity of policy
action, with population density and the degree of trust in government also important.
Governments freed up additional resources to strengthen health system responses
to COVID‑19
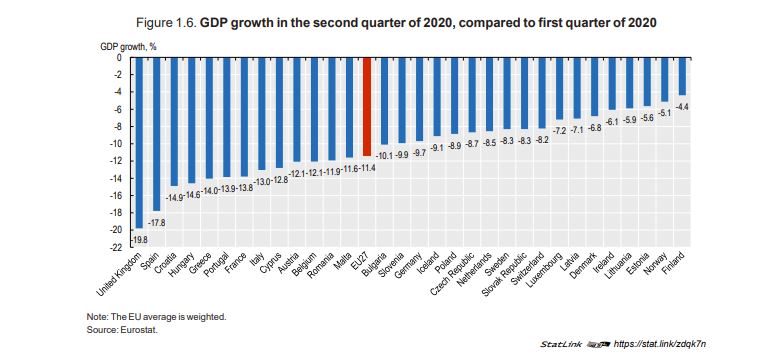
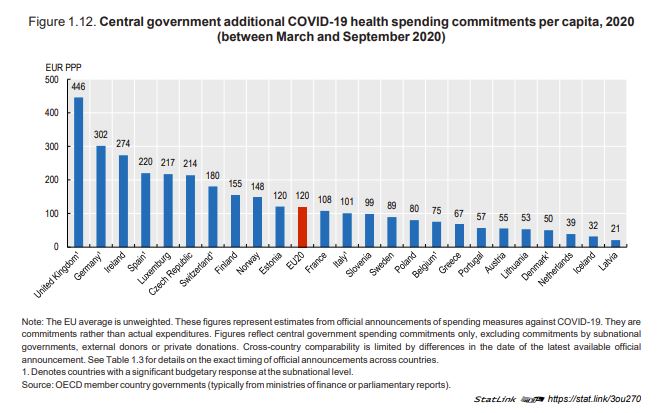
Governments put together substantial financial packages to respond to the COVID‑19 pandemic.
These resources were used to protect people’s jobs and businesses, as well as to strengthen health
system responses to COVID‑19. Across European countries, most fiscal responses – including direct
budgetary measures related to spending and revenue policies, alongside other interventions such as
loans, equity injections and government guarantees – amounted to between 5‑20% of GDP.
The health sector was naturally among the first recipients of additional financial resources.
Amongst European countries with comparable data, central government budgetary commitments to
health system responses to COVID-19 ranged from almost EUR 450 per person in the United
Kingdom, and around EUR 300 per person in Germany and Ireland, to under EUR 50 per person in
Latvia, Iceland and the Netherlands, adjusted for purchasing power parity (Figure 1.12).
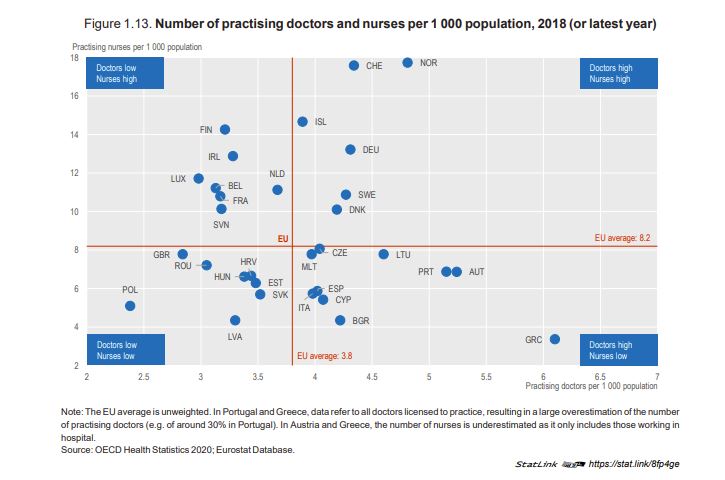
Health professionals have been at the forefront of the response to the COVID‑19
outbreak
As doctors, nurses and other health professionals mobilised on the frontline to respond to the pandemic, health systems sought ways to increase the number of staff available during the peak of the pandemic and to make the most efficient use of their work.
Some health systems lacked sufficient hospital beds, equipment, supplies and
medicines to treat COVID‑19 patients, but policies to boost surge capacity have
helped
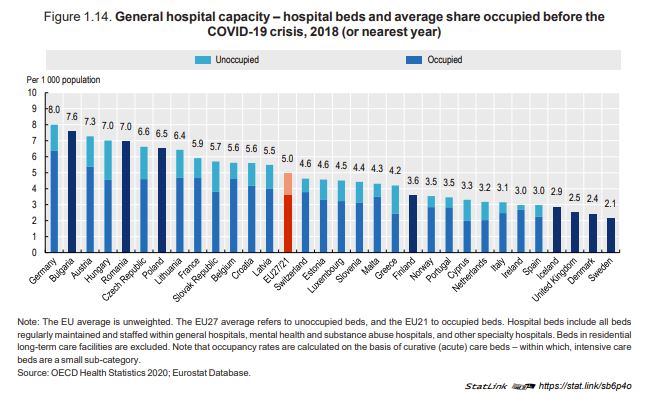
Hospitals have often been placed under immense strain, but governments found innovative
solutions to increase surge capacity, particularly for intensive care units.
While the pandemic has put all health services under severe strain, its impact on hospitals has
been particularly drastic. In this context, having a high number of beds per population is a useful
general proxy of the capacity of hospitals to meet surges in demand (Figure 1.14). In terms of existing
capacities, Germany had the most hospital beds per capita in 2018, with eight beds per 1 000
population, followed by Bulgaria and Austria. Most European countries have between three and seven
hospital beds per 1 000 population, but numbers are lower in Sweden, Denmark, Iceland and the
United Kingdom.
Obtaining the necessary equipment, supplies and medicines has proven challenging, particularly early in the crisis
Alongside beds (both general, acute and ICU beds), hospitals and other health facilities require
sufficient medical equipment, supplies and medicines. Personal Protective Equipment (PPE),
ventilators, infusion pumps, monitoring and laboratory equipment, and certain medicines (notably
anaesthetics, antibiotics, muscle relaxants, resuscitation medicines and anti-diuretics; as well as
medical oxygen) are some critical items needed to treat COVID‑19 patients.
However, purchasing and distributing such items under conditions of extreme urgency and uncertainty is challenging – with risks of shortfalls in supply or poor quality products due to disruptions in the global supply chain. Even before the onset of the pandemic, countries have reported increased shortages of critical medical supplies and products. For example, across a sample of 14 OECD countries, the number of notifications of expected or actual medicine shortages grew by more than 60% between 2017 and 2019.
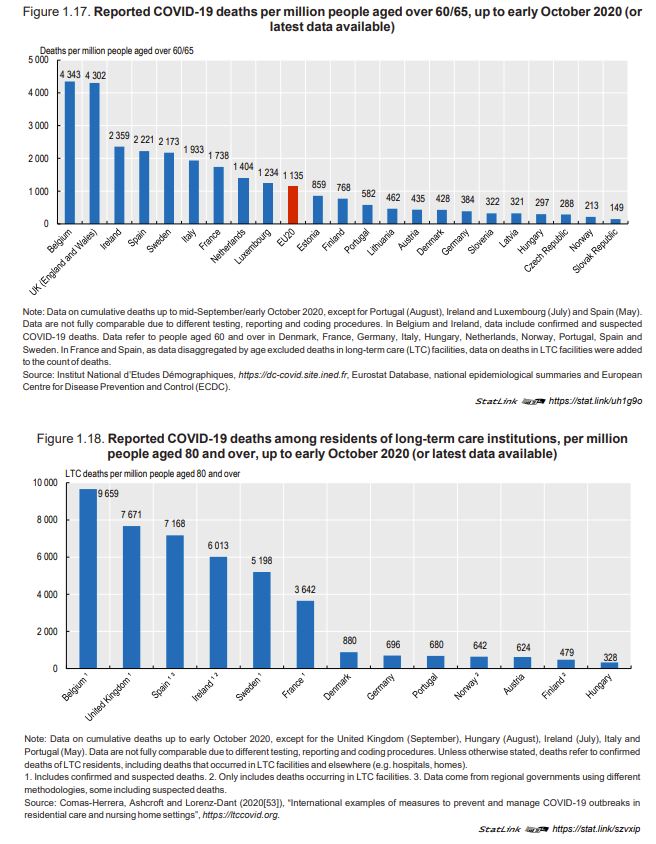
Almost all reported COVID‑19 deaths have been amongst those aged 60 and above, with recipients of long-term care particularly at risk
While COVID‑19 has claimed the lives of many people across all age groups, people with
comorbidities (e.g. obesity, cardiovascular diseases) and in particular older populations face an
elevated risk of dying from COVID‑19. Among 22 European countries with data available by age
group, reported COVID‑19 deaths per million people aged 60/65 and over were on average 3.7 times
higher than amongst the population as a whole. In nearly all of these countries, 90% or more of
reported COVID‑19 deaths were amongst people aged 60/65 and over; with people aged 80 and over
accounting for around half of all COVID‑19 deaths.
The United Kingdom, Italy, Spain and France all reported more than 17 000 deaths amongst
those aged 60 and over (as of mid-September). Adjusting for population size, reported COVID‑19
mortality rates amongst people aged 60/65 and over were more than 3 000 deaths per million people
in this age group in the United Kingdom (England and Wales) and Belgium, and over 1 000 deaths
per million people in Ireland, Sweden, Italy, Spain, France and the Netherlands (Figure 1.17). Mortality
rates were even higher amongst those aged 80/85 and over, reaching over 10 000 reported deaths
per million people in this age group in the United Kingdom (England and Wales), Belgium and Ireland.
COVID‑19 has adversely affected patients with other health care needs
COVID‑19 has had a major indirect health impact on patients who did not contract the virus.
Acute and chronic care patients have faced disruptions to essential care, in terms of delayed
diagnoses, foregone care and impeded continuity of care. This contributes to worse health outcomes
for many people, now and in the future. A dual-track approach is therefore needed to maintain high
quality care for non-COVID‑19 acute and chronic care, alongside boosting surge capacity to combat
the virus.
- COVID‑19 has led to postponed elective surgeries, fewer visits to emergency departments
and less use of outpatient services, affecting both acute and chronic care patients - Delays in cancer diagnoses and treatments are likely to increase cancer deaths
Strengthened primary care systems are key to maintaining continuity of care for nonCOVID‑19 patients
The emerging evidence described above points to the risks of not giving sufficient weight to non-COVID‑19 health care needs, resulting in urgent health problems remaining undiagnosed and
exacerbated chronic illnesses. Maintaining primary health care practices, establishing community
care facilities, extending home-based programmes, expanding the role of primary health care workers
and increasing telemedicine consultations are key to minimise delays and forgone care for all
patients.
- Primary health care practices, community care facilities and home-based programmes help maintain access to routine care
- Mobilising community pharmacists helps ensure patients continue to get needed medicines
- Telemedicine has helped preserve continuity of care while containing the spread
Countries maintained access to mental health services under difficult
circumstances, and are starting to respond to emerging mental health needs
The COVID‑19 crisis has had a marked impact on the mental health of both people with preexisting mental health conditions and the general population. Countries have taken decisive action to
preserve some access to mental health support. Many countries have also been providing well-being
support to the general population, for example through online advice or phone hotlines. Nonetheless,
the combination of reduced capacity in mental health services and increased demand caused by the
worsening mental health status of the general population, risks putting additional strain on mental
health services which were already over-stretched in many countries.
- People living with mental health conditions did not always get the care they need
- Emerging needs – the COVID‑19 crisis has increased levels of mental distress
- Innovative policies have helped protect population mental well-being
- Countries have sought to protect access to care for people with mental health conditions,
including inpatient care where necessary
Testing the resilience
The COVID‑19 pandemic has therefore put an immense strain on European countries, testing
the resilience of every country’s government and people. It has also tested the ability of EU Member
States and the European Commission to develop a co‑ordinated set of responses to a common threat
(European Commission, 2020).
Based on this review, the chapter draws out policy insights that are likely to contribute to better preparedness and more effective responses to the evolving pandemic and future health threats. As the data and evidence are still developing, results from this chapter are “initial findings”, not a definitive review.
Defining health systems resilience
The concept of resilience has been applied to shocks and disruptive events such as epidemics, economic crises and environmental disasters. It recognises the importance of risk management, but also that absolute prevention avoidance of shocks such as COVID‑19 is impossible given the unpredictable nature of systemic threats. Resilience is therefore seen to be as much about recovery and adaption, as it is about prevention and avoidance. Building on these conceptual analyses, the focus of this chapter is predominantly on the capacity of European countries’ health systems to absorb and adapt to the shock of COVID‑19.
“Resilience acknowledges that massive disruptions can and will happen – in future, climate disruption will likely compound other shocks like pandemics – and it is essential that core systems have the capacity for recovery and adaptation to ensure their survival, and even take advantage of new or revealed opportunities following the crises to improve the system through broader systemic changes… The new approach to resilience will focus on the ability of a system to anticipate, absorb, recover from, and adapt to a wide array of systemic threats. Health system resilience describes the capacity of a health system to (a) proactively foresee, (b) absorb, and (c) adapt to shocks and structural changes in a way that allows it to (i) sustain required operations, (ii) resume optimal performance as quickly as possible, (iii) transform its structure and functions to strengthen the system, and (possibly) (iv) reduce its vulnerability to similar shocks and structural changes in the future” (EU Expert Group on HSPA, 2020)
(OECD 2020) Tweet
Improvements of the resilience of health systems to the ongoing pandemic and future health crises - emerging insights
COVID‑19 has had a huge and lasting impact in Europe and worldwide, testing the resilience of
health systems and placing immense pressure on health workers. The virus spread rapidly across
Europe, leading to many deaths and stringent containment policies by a large number of countries in
an attempt to contain the outbreak.
- If countries are prepared and are able to act quickly, they may be able to avoid costly
containment and mitigation measures - Adaptive surge capacity can help treat COVID‑19 patients in an effective manner, but
countries will also need to invest more in their health workforce - Strong primary health care and mental health services are needed for COVID‑19
patients and to maintain high quality care for non-COVID‑19 patients - Vulnerable populations need much more support in the health system and beyond
- Health resilience is a multi-system challenge that requires close international
cooperation
Citation:
OECD/European Union (2020), Health at a Glance: Europe 2020: State of Health in the EU Cycle, OECD Publishing, Paris, https://doi.org/10.1787/82129230-en