This chapter describes the health status of EU citizens, including trends in life expectancy, the main causes of death, health inequalities, the occurrence of communicable and chronic diseases, and mental health issues. It shows modifiable risk factors to health, including smoking, alcohol consumption, illicit drug use, unhealthy nutrition, lack of physical activity and obesity. Moreover, this article looks at recent trends in health spending, both at an overall level but also disaggregated by type of health service and by health care provider.
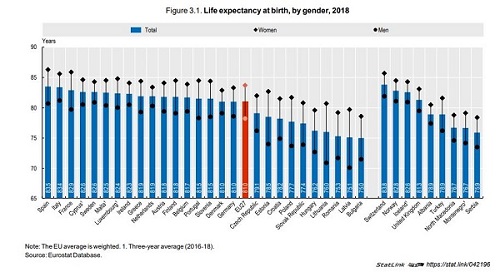
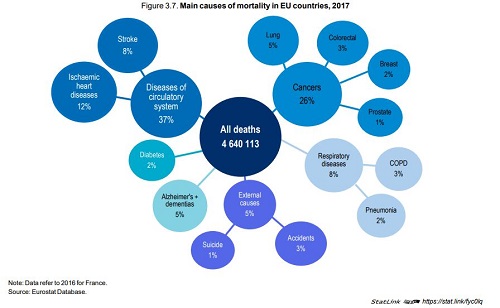
Life expectancy now reaches 81 years in the EU as a whole, but the gains have slowed markedly in several Western European countries in recent years due to severe flu seasons and a slowdown in reductions in cardiovascular mortality. The COVID‑19 pandemic will result in a further stagnation or even reduction in life expectancy in 2020 in those countries that have been most impacted. The main causes of deaths across EU countries remain cardiovascular diseases (over 1 700 000 deaths in 2017) and cancers (1 200 000 deaths), which together account for over 60% of all deaths. Large inequalities in life expectancy persist by gender and socio-economic status. On average across EU countries, 30‑year‑old men with a low education level can expect to live about seven years less than those with a university degree or the equivalent.
This education gap among women is smaller, at about three years. At age 65, men and women across EU countries could expect to live over 75% of their remaining years of life free of disability in 2018. Nearly 40% of people aged 65 and over report having at least two chronic conditions, although this does not necessarily impede them from leading a normal life. About 30% of people aged 65 and over report at least one limitation in (instrumental) activities of daily living that may require some long-term care assistance.
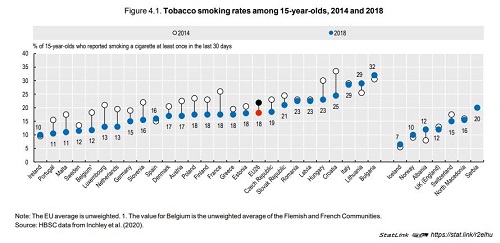
Despite progress in reducing smoking rates over the last decades, about one‑fifth of adults still smoke every day and tobacco consumption remains the largest behavioural risk factor to health, accounting for about 700 000 deaths per year across EU countries. Alcohol consumption is responsible for another 255 000 to290 000 deaths per year across EU countries.
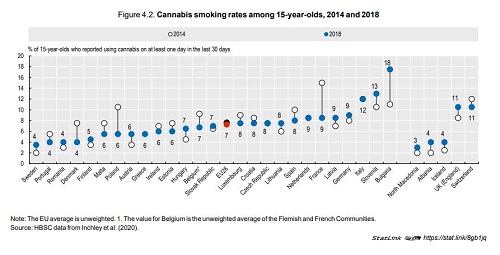
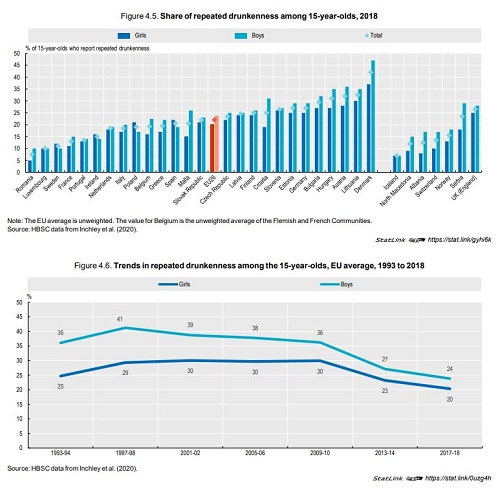
While alcohol control policies have achieved progress in reducing overall alcohol consumption, heavy alcohol consumption remains an issue among a sizeable share of adolescents and adults: more than one in five adolescents aged 15 report having been drunk more than once in their life and one‑third of adults report regular heavy drinking. The use of illicit drugs is another important public health issue in Europe: about 15% of young people aged 15 to 34 report having used cannabis in the last year. Weight problems are widespread in most EU countries, with nearly one in five adolescents overweight or obese on average across EU countries in 2018 and more than one in six adults obese. Overweight and obesity is driven by unhealthy nutrition habits and lack of physical activity. Only one in seven 15‑year-olds on average across EU countries report doing at least moderate physical activity at least one hour daily, and less than half report eating at least one fruit or vegetable per day. Large socio-economic inequalities exist for most risk factors to health. For example, overweight and obesity rates among children and adolescents are 50% greater among those living in the least affluent families than those living in the most affluent.
A particular focus is on analysing spending on primary health care and pharmaceuticals. This section also analyses how health care is financed in Europe, both in terms of the type of financing arrangements in place and the revenues that ultimately fund health spending.
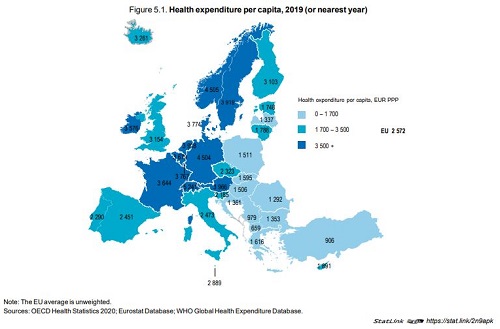
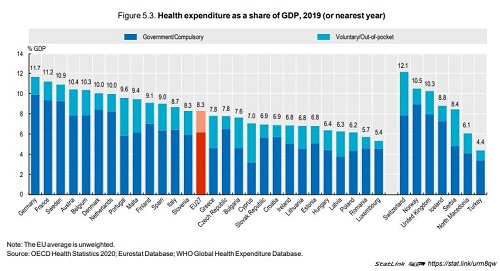
In 2019, health spending across EU countries stood on average at 8.3% of GDP, ranging from over 11% in Germany and France to less than 6% in Luxembourg and Romania. This share remained largely unchanged from previous years as health spending grew in line with the economy but it can be expected that the COVID‑19 pandemic will lead to an increase of the health spending share of GDP in many countries in 2020. On a per capita basis, there is a three‑fold difference between the EU countries in Western and Northern Europe that spend the most on health (Germany, Austria, Sweden and the Netherlands) and those in Central and Eastern Europe that spend the least (Romania, Bulgaria, Latvia and Croatia).
In most countries, payments for curative and rehabilitative care services make up the bulk of health spending, while spending on pharmaceuticals also account for a large share of health expenditure particularly in some Central and Eastern European countries.
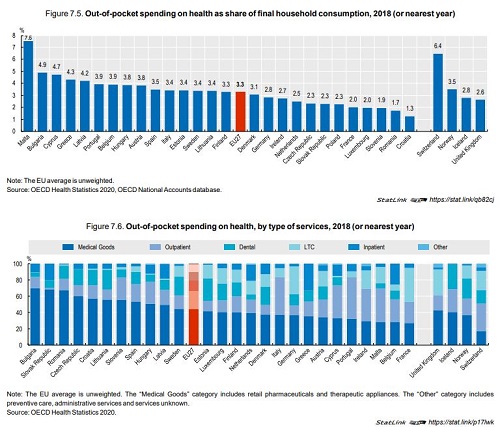
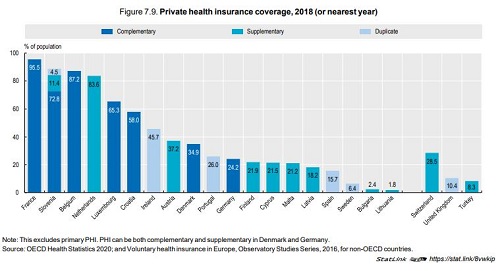
Regarding the financing of health care, compulsory schemes, either government financed or through compulsory public or private health insurance, account for nearly three‑quarters of overall health spending on average across EU countries. However, outof-pocket expenditure also plays an important role in health financing in several Southern as well as Central and Eastern European countries.
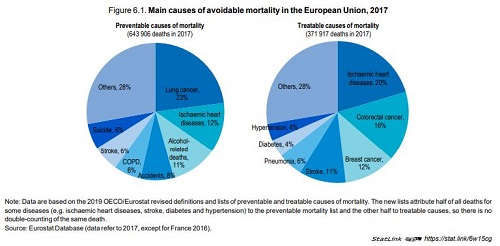
In 2017, more than 1 million people in EU countries died prematurely from diseases and injuries that could potentially have been avoided through more effective public health policies or health care.
The main causes of avoidable mortality include ischaemic heart diseases, lung cancer and accidents.
Vaccination rates among children and older people have decreased in several countries in recent years following anti-vaccination campaigns and a belief that vaccination might not be needed. It is important to tackle vaccine hesitancy and improve vaccination coverage to reduce the spread of communicable diseases that can be effectively prevented through vaccines and the burden on health systems.
Progress has been made in tackling cancer in many countries through the implementation of population-based screening programmes to detect cancer earlier and the provision of effective and timely cancer care. These efforts have led to increased survival following diagnosis and reduced mortality from cancer in most countries, yet wide disparities in cancer care persist across countries. Promoting more patient-centered care has become a growing priority across EU countries in recent years to improve the quality of care and responsiveness to patients’ expectations.
Based on surveys seeking patient-reported experience measures (PREMs), citizens in most countries rate the quality of primary care high. These survey results signal clearly the importance of good provider/patient communication and patient involvement in care and treatment decisions.
Most EU countries have achieved universal coverage for a core set of health services, although the range of services covered and the degree of cost-sharing vary. Effective access to care can be restricted for financial reasons, but also because of health workforce shortages, long waiting times or long distance to travel to the closest health care facility.
In most EU countries, only a small share of the population reported unmet needs for health care in 2018, but this proportion was higher among low-income households, mainly for financial reasons. On average across EU countries, around a fifth of all health spending is paid out-of-pocket by households, but with wide variations across countries.
In general, countries that have a higher share of out-of-pocket spending also have a higher proportion of the population facing catastrophic out-of-pocket payments for health services, particularly among low-income groups. Although the number of doctors and nurses per population has increased over the past decade in nearly all EU countries, shortages persist in many countries and were brought to light during the COVID‑19 pandemic. Long waiting time for some health services such as elective surgery is an important policy issue in many EU countries, as it restricts timely access to care and generates patient dissatisfaction. Even before the COVID‑19 pandemic, waiting times for elective surgery were on the rise in many countries as the demand for surgery was increasing more rapidly than the supply.
Citation:
OECD/European Union (2020), Health at a Glance: Europe 2020: State of Health in the EU Cycle, OECD Publishing, Paris, https://doi.org/10.1787/82129230-en
Published in GI-Mail 03/2020 & 04/2021 (English & German edition).
- Do you already know our monthly newsletter GI-Mail with useful tips on postgraduate courses?
Sign up here. - Are you looking for vacancies or new career challenges? Here you will find the latest vacancies and job offers.
- Do you already know our monthly job-information GI-Jobs with current job offers for doctors, managers and nurses? Sign up here.
- Are you interested in up to date postgraduate courses and CME? In our education database »medicine & health« you will find new education events from over 2300 organizers.