August 2025.
Opioid overdose continues to be one of the most urgent public health threats of our time. Despite the fact that effective treatments and preventive measures exist, hundreds of thousands of lives are lost every year due to misuse, dependence, and overdose. Drawing on the latest WHO data, this article provides medical professionals with an updated overview of the issue, highlighting clinical features, risk factors, and strategies for effective prevention and response.
What Are Opioids?
Opioids include naturally occurring compounds from the poppy plant (Papaver somniferum), as well as semisynthetic and synthetic substances that act on opioid receptors in the brain. They are indispensable in medicine, providing analgesic and sedative effects, and remain essential in pain and palliative care.
Common examples include morphine, codeine, tramadol, fentanyl, methadone, and buprenorphine. However, illicitly manufactured opioids such as heroin, or counterfeit versions of prescription drugs containing fentanyl analogues, are fueling a parallel crisis.
Beyond their medical value, opioids produce euphoria, which contributes to their non-medical use and makes them highly addictive.
The Global Burden
Drug use continues to take a heavy toll worldwide. In 2021, nearly 296 million people used drugs, with 60 million using opioids. About 39.5 million people were living with drug use disorders.
In 2019 alone, approximately 600,000 deaths were attributed to drug use; opioids were involved in close to 80% of these cases. Of those, about 125,000 deaths were caused directly by opioid overdose.
The burden has been rising in many countries, driven by increased prescription opioid availability, as well as the spread of highly potent synthetic opioids such as fentanyl. The COVID-19 pandemic amplified this trend, particularly in North America, where overdose deaths surged dramatically.
Recognizing Opioid Overdose
Clinically, opioid overdose can be identified by the well-known triad:
- pinpoint pupils
- unconsciousness
- respiratory depression
These signs demand immediate recognition, as the progression from overdose to respiratory failure and death can be rapid.
Risk Factors
Certain situations markedly increase the risk of overdose. These include opioid use disorder, injecting opioids, and resuming use after a period of abstinence, such as after incarceration or detoxification. Patients on high daily doses of opioids, or those using them in combination with alcohol, benzodiazepines, barbiturates, or anesthetics, are also at elevated risk.
Concurrent health conditions HIV, liver disease, lung disease, or mental health disorders further exacerbate vulnerability. Demographically, men, older individuals, and those with lower socioeconomic status face disproportionately higher risk.
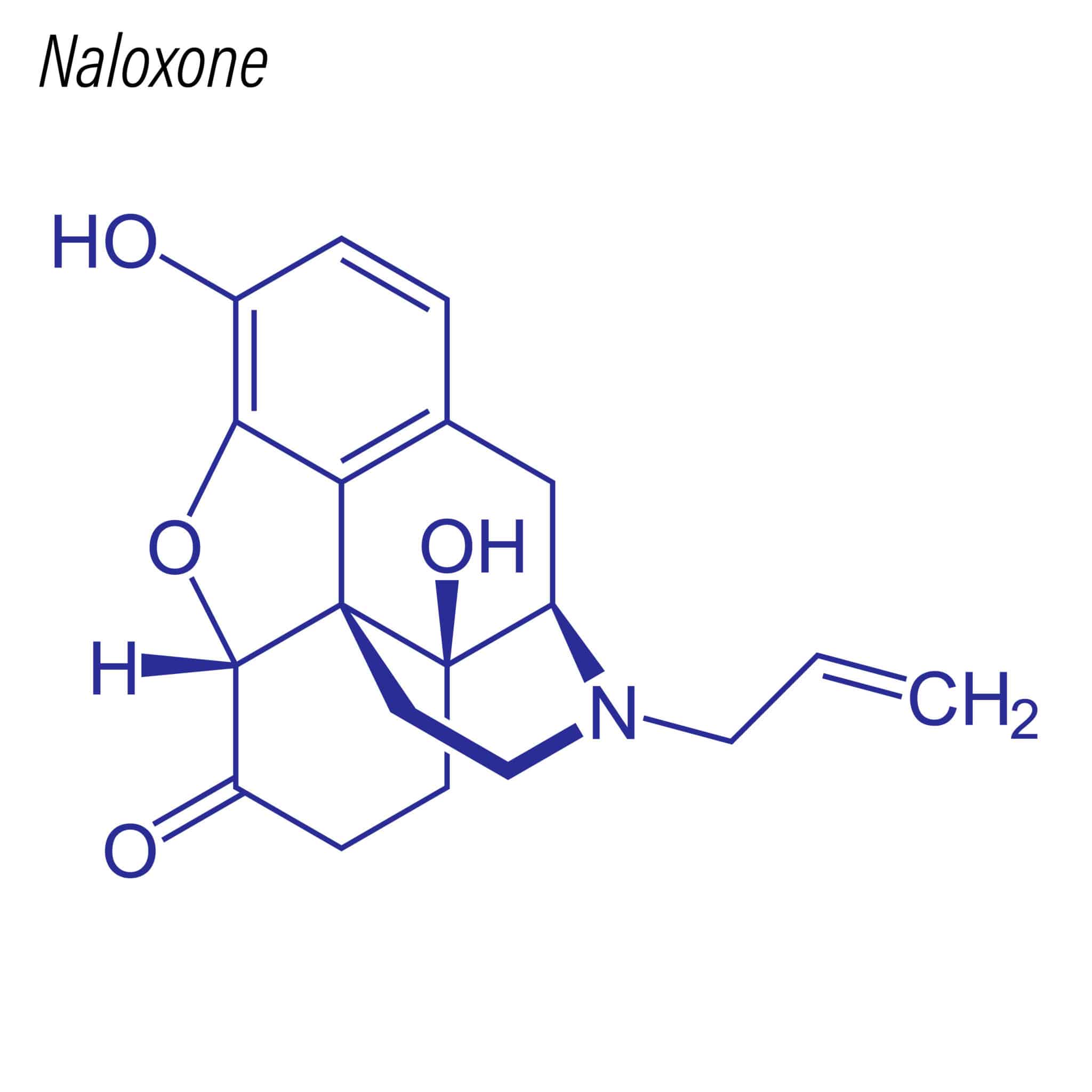
Emergency Response and Naloxone
Opioid overdose deaths are preventable. The antidote, naloxone, can reverse respiratory depression if administered quickly. Importantly, naloxone has minimal to no effect in individuals who have not taken opioids, making it a safe intervention.
Despite its effectiveness, access to naloxone remains limited in many countries, often restricted to health-care providers. Encouragingly, some nations including Australia, Canada, Italy, the UK, and Ukraine have made naloxone available without prescription.
Community distribution programs, especially when paired with training, have proven highly effective in reducing fatalities.
Prevention Strategies
Preventing opioid overdose requires both systemic and clinical interventions. Key measures include:
- Expanding access to treatment for opioid dependence, particularly with methadone and buprenorphine.
- Promoting rational and evidence-based prescribing of opioids.
- Monitoring prescribing and dispensing patterns to detect misuse.
- Restricting inappropriate over-the-counter sales.
- Empowering communities by training family members, peers, and service providers in naloxone use and overdose recognition.
Yet, the gap between recommendation and practice remains large: fewer than 10% of people worldwide who need treatment for opioid dependence are currently receiving it.
For more information visit the website of the WHO.
Published in GI-Mail 09/2025 (English edition).
- Do you already know our monthly newsletter GI-Mail with useful tips on postgraduate courses?
Sign up here. - Are you looking for vacancies or new career challenges? Here you will find the latest vacancies and job offers.
- Do you already know our monthly job-information GI-Jobs with current job offers for doctors, managers and nurses? Sign up here.
- Are you interested in up to date postgraduate courses and CME? In our education database »medicine & health« you will find new education events from over 2300 organizers.