In the past year, measles has returned to Europe with a force few expected. From April 2024 to March 2025, over 26,000 cases were reported across EU/EEA countries: The vast majority among people who had not been vaccinated. Romania alone accounted for more than 21,000 cases, while Italy, France, Germany, and Belgium all saw surges. Even more alarming: over 85% of all infected individuals were unvaccinated.
It’s moving through schools, hospitals, and communities, revealing deep cracks in Europe’s public health defences.
For many, this may come as a shock. After all, measles is one of the most preventable infectious diseases in the world. A safe, effective vaccine has been in routine use for decades. And yet, due to gaps in immunisation coverage, missed doses during the COVID-19 pandemic, misinformation, and structural healthcare barriers, the virus has once again found fertile ground – especially among young children and adults over thirty.
A Closer Look at the Numbers
Between April 2024 and March 2025, the European Centre for Disease Prevention and Control (ECDC) recorded the following:
- 26,222 measles cases reported in the EU/EEA
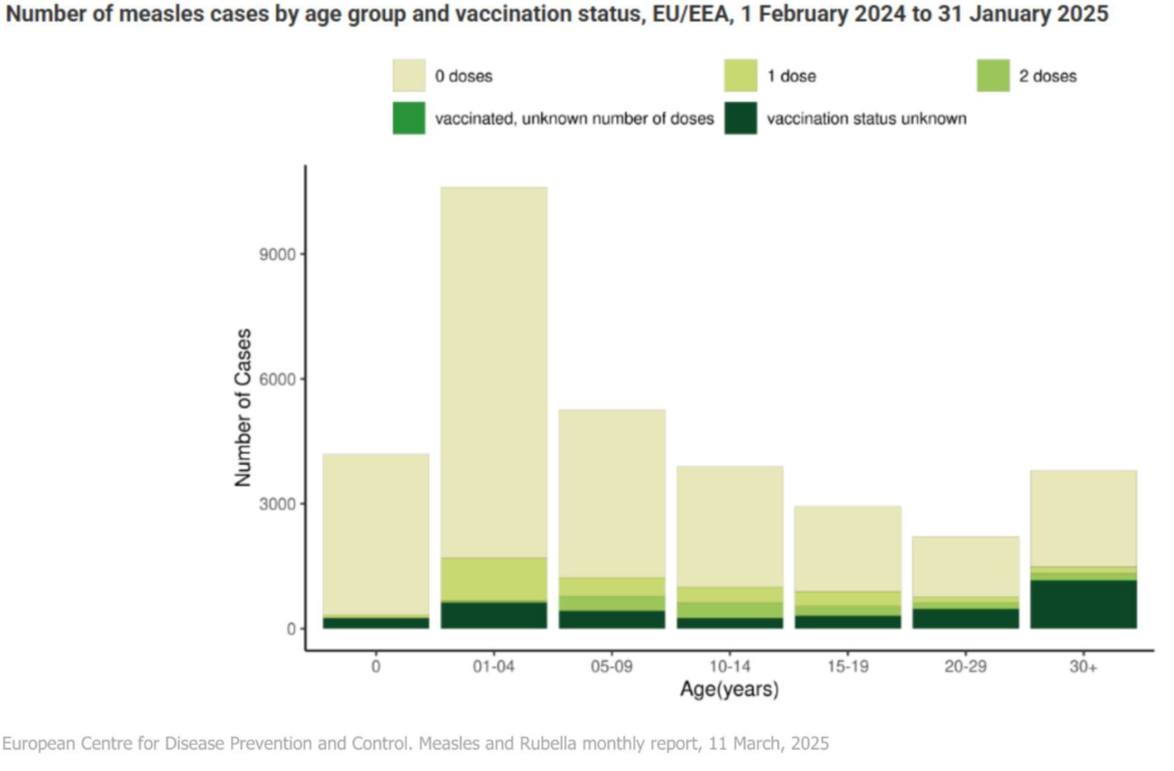
- 85.8% of those infected were unvaccinated
- 9.0% had received only one dose of the vaccine
- 4.8% were fully vaccinated with two or more doses
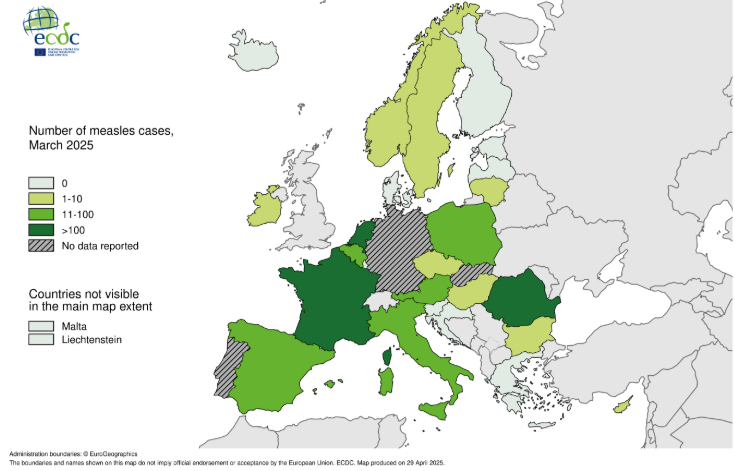
Among the hardest-hit countries:
- Romania: 21,620 cases
- Italy: 1,026
- France: 695
- Germany: 560
- Belgium: 540
When looking at age groups, the virus hit the youngest and the oldest children hardest:
- 44.4% of cases occurred in children under five years old
- 27.7% were aged 15 years or older
- Infants under one year had the highest notification rate: 849.7 cases per million
Fourteen measles-related deaths were reported during this period – 13 in Romania and one in France. These are not numbers from countries with limited access to healthcare or vaccines. These are EU member states, and the cause is preventable.
A Virus That Doesn’t Wait
Measles remains one of the most contagious viruses on earth. It spreads through respiratory droplets such as coughing, sneezing, even breathing and can remain infectious in the air or on surfaces for up to two hours. It often transmits before symptoms even appear.
Early signs include fever, cough, runny nose, and conjunctivitis. A few days later, the characteristic rash appears, spreading from the hairline downward. But while the rash signals infection, the real danger lies in the complications: pneumonia, ear infections, brain swelling (encephalitis), and, in rare cases, a fatal degenerative condition called SSPE that can appear years later.
Children under five and immunocompromised individuals are particularly at risk. In fact, the majority of deaths in recent outbreaks involved unvaccinated children, those too young to receive the vaccine or whose parents delayed or declined immunisation.
Immunisation: Why Two Doses Matter
The measles vaccine, typically administered as part of the MMR (measles, mumps, rubella) combination, is remarkably effective. Two doses are required to ensure full protection:
- The first dose, usually given at 12 – 15 months of age, provides immunity to around 95% of recipients
- A second dose, administered between 3 – 7 years, boosts immunity close to 100%
Despite this, most EU/EEA countries have not met the 95% coverage threshold required for herd immunity. As of 2023, only Hungary, Malta, Portugal, and Slovakia had achieved this for both doses.
Gaps in vaccination coverage don’t just affect children. Many adults over 30 either received only one dose or were never vaccinated. Others assume they’re protected but have no records to confirm it. These individuals are now contributing significantly to the spread.
What Needs to Happen Now
According to the ECDC, the current trend is likely to continue, with a further rise in cases expected in spring 2025. Action is urgently needed at every level: individual, medical, and governmental.
Efforts must focus on:
- Closing immunity gaps in adolescents and adults
- Expanding catch-up programmes for those who missed routine vaccinations
- Educating healthcare providers to check vaccination status and recognize early symptoms
- Strengthening surveillance and outbreak response capacity
- Promoting vaccine acceptance through targeted communication strategies
- Ensuring access for underserved and vulnerable groups
Healthcare professionals are also urged to lead by example, by ensuring they themselves are vaccinated.
What You Can Do
You don’t have to wait for a government campaign. Start with these simple but crucial steps:
- Check your vaccination status. If you’re unsure, speak with your doctor.
- Make sure your children have received both doses of the MMR vaccine.
- If you plan to travel, ensure your MMR vaccination is up to date. It needs at least two weeks to become effective.
- Watch for symptoms, and seek medical advice immediately if measles is suspected.
- Don’t delay. In outbreak situations, every day, every dose, matters.
What Makes Measles Eradicable?
Unlike many infectious diseases, measles meets the scientific criteria for complete eradication. Hence the virus could be eliminated globally with sustained public health effort.
This is possible because:
- Humans are the only host: Measles has no animal or environmental reservoir.
- Reliable diagnostic tools exist: Laboratory confirmation and genomic sequencing can pinpoint cases and identify viral lineages.
- The vaccine is highly effective and safe: Two doses of a measles-containing vaccine provide lifelong protection in nearly all recipients.
- Immunity is sterilizing: Once protected, reinfection is rare and those who recover naturally also gain strong immunity.
Surveillance across Europe is coordinated via ECDC’s Epipulse platform, with 30 EU/EEA countries submitting case-based measles data monthly. Genomic analysis of virus strains has helped trace outbreaks back to importation events and pinpoint immunity gaps.
Still, reliable data requires timely reporting, standardized case definitions, and adequate diagnostic capacity. These challenges remain uneven across the region. In some countries, measles cases are still underdiagnosed or underreported, particularly where laboratory testing is limited or symptoms are misattributed to other viral infections.
This reinforces the importance of high-quality, active surveillance, especially in times of rising transmission.
A Preventable Tragedy
The return of measles is not an inevitability, it’s a consequence of inaction. Measles meets all the criteria for eradication: no animal host, reliable testing, and a proven vaccine. Yet the virus continues to exploit gaps in our defences.
This is a solvable crisis. But solving it requires remembering what was almost forgotten: vaccines work but only if they’re used.
Published in GI-Mail 06/2025 (English edition).
- Do you already know our monthly newsletter GI-Mail with useful tips on postgraduate courses?
Sign up here. - Are you looking for vacancies or new career challenges? Here you will find the latest vacancies and job offers.
- Do you already know our monthly job-information GI-Jobs with current job offers for doctors, managers and nurses? Sign up here.
- Are you interested in up to date postgraduate courses and CME? In our education database »medicine & health« you will find new education events from over 2300 organizers.